Cervical cancer
What is cervical cancer? (Cause / occurrence / progress)
Cervical cancer is cancer that begins at the entrance to the uterus. There are two types of epithelium that cover the surface of the cervix: squamous epithelial cells and columnar epithelial cells (glandular cells), and cervical cancer mainly develops near the boundary between these two types of cells. This borderline is affected by the follicular hormone (estrogen) and is located near the entrance to the cervix during maturity, but moves into the cervix at the back of the cervix during old age. As a result, it can be difficult to detect cancer with the naked eye in old age.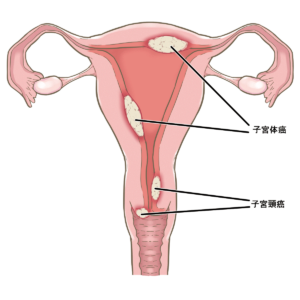
Cervical cancer can be broadly divided into "flat epithelial cancer" that develops in squamous epithelial cells and "adenocarcinoma" that develops in columnar epithelial cells. Adenocarcinoma has recently increased and accounts for about 20%, and it is difficult to detect compared to squamous cell carcinoma, lymph node metastasis is likely to occur from the beginning, and radiation therapy and chemotherapy are difficult to treat, so it is a difficult cancer to treat.
▶進行と生存率
子宮頸がんの発生原因として、ヒトパピローマウイルス(HPV)の持続感染が明らかになりました。子宮頸がん予防ワクチンは本邦でも9価HPVワクチンまで承認されており、HPVワクチン接種を国のプログラムとして早期に取り入れたオーストラリアでは、HPVワクチン接種と子宮頸がん検診によって2028年に世界に先駆けて新規の子宮頸がん患者がほぼいなくなるとのシミュレーションがなされました。HPVワクチンが定期接種化されているにもかかわらず積極的勧奨が中断されている日本においては、性交開始年齢の若年化に伴い子宮頸がんが若い女性に急増しています。また、喫煙も子宮頸がんの発生を高める要因と考えられています。
Reprinted from "National Cancer Center Cancer Information Service" https://ganjoho.jp/public/cancer/cervix_uteri/treatment.html
Created from "Guidelines for Treatment of Cervical Cancer, Uterine Body Cancer, and Ovarian Cancer for Patients and Their Families, 2nd Edition (2016)" (Kanahara Publishing), edited by the Japanese Society of Gynecologic Oncology
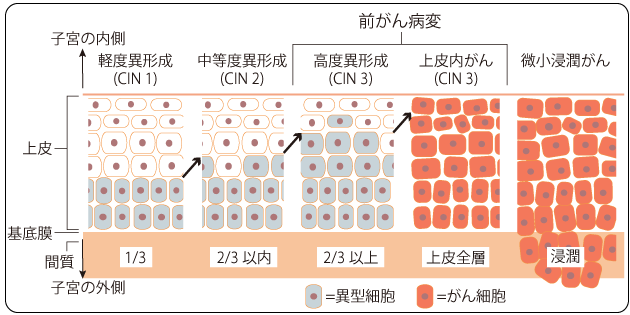
Squamous epithelial cancer develops and progresses according to the flow shown in the above figure. Most of the HPV infections are eliminated by the immune system, but some are said to be persistently infected and develop cancer over 5 to 10 years.
It is thought that about 1 in 1000 people with HPV will progress to invasive cancer.
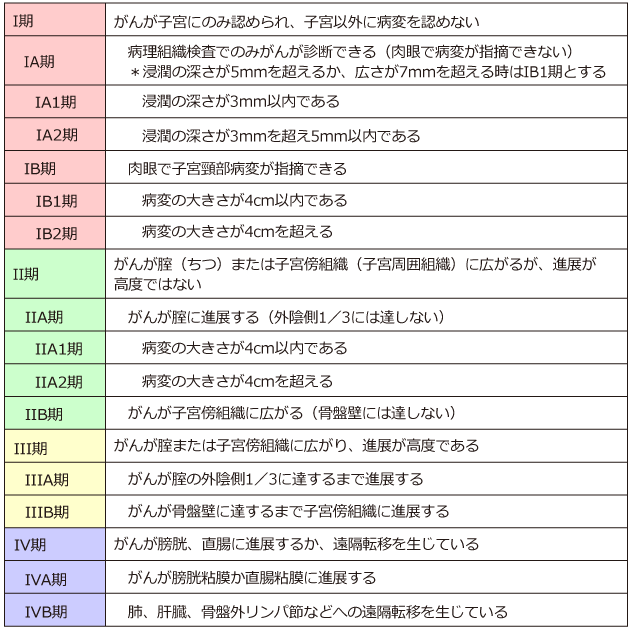
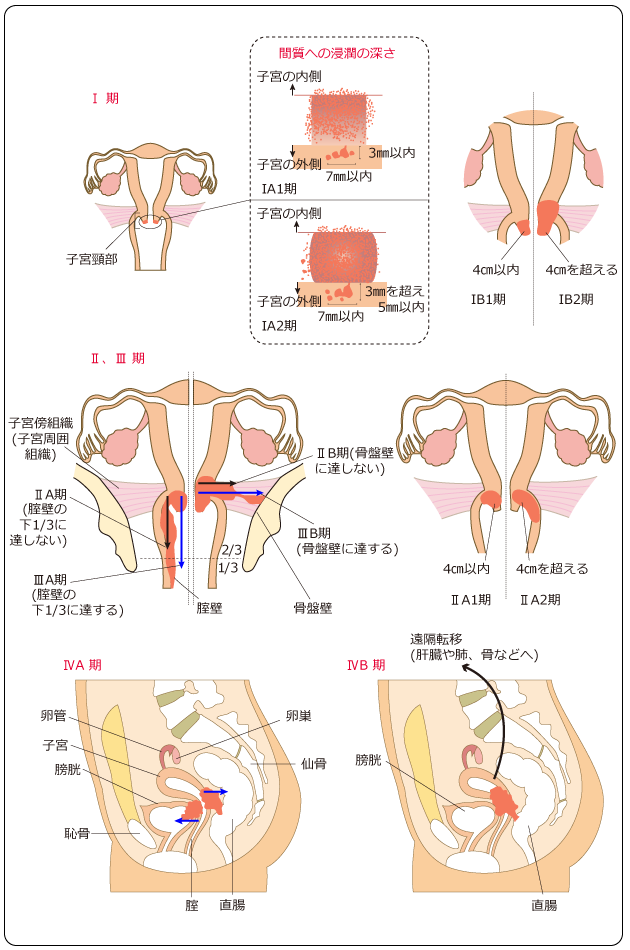
Advanced stage classification of cervical cancer
Excerpt from "National Cancer Center Cancer Information Service" https://ganjoho.jp/public/cancer/cervix_uteri/treatment.html
Created from "Cervical Cancer Handling Regulations, Pathology Edition, 4th Edition (2017)", p.10 (Kanahara Publishing), edited by the Japanese Society of Obstetrics and Gynecology and the Japanese Society of Pathology
Excerpt from "National Cancer Center Cancer Information Service" https://ganjoho.jp/public/cancer/cervix_uteri/treatment.html
Created from "Guidelines for Treatment of Cervical Cancer, Uterine Body Cancer, and Ovarian Cancer for Patients and Their Families, 2nd Edition (2016)" (Kanahara Publishing), edited by the Japanese Society of Gynecologic Oncology
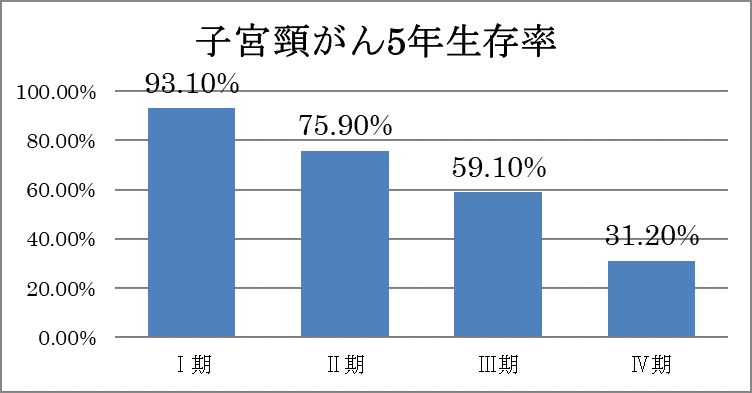
2020 Japan Society of Obstetrics and Gynecology Gynecologic Oncology Committee Report 5-year survival rate
Diagnostic method
Cervical cancer screening is called a screening test and should be taken by any adult woman with or without symptoms. The inspection result is as shown in the figure below. If it is not negative, you should immediately go to a gynecological institution for a detailed examination.
Depending on the type of abnormality, HPV virus test may be performed, or colposcopy (vaginal magnifying glass) and tissue biopsy may be performed.
Classification of cervical cancer cytology based on Bethesda system (flat epithelial cells)
-6-1024x632.jpg)
From the revised "Cervical Cytology Report Form Based on Bethesda System 2014" by the Obstetrics & Gynecology
If you find out that you have cancer, you can inspect and palpate the spread of the cancer, perform endoscopy such as cystoscope and colonoscopy, and perform imaging tests such as CT and MRI. The advanced stage of cervical cancer is diagnosed before surgery.
Method of treatment
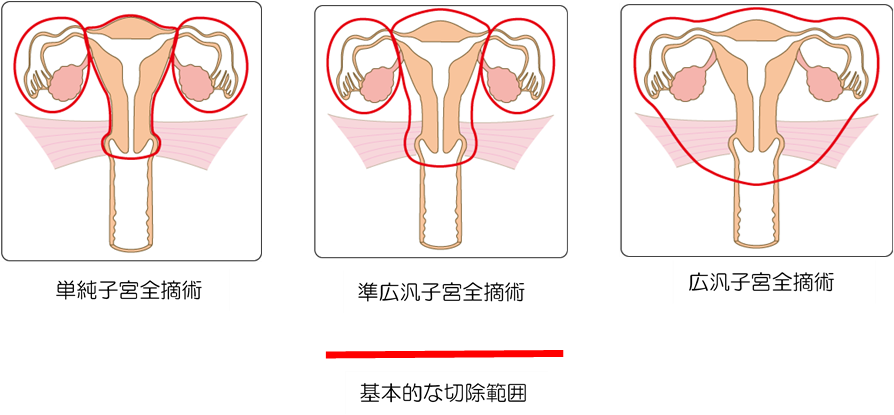
Carcinoma in situ is mostly cured by cervical conization, which cuts the cervix into a conical shape, but it is an intraepithelial adenocarcinoma with a higher risk of recurrence than carcinoma in situ of the uterus, or there is no hope of pregnancy. In this case, a simple total hysterectomy may be performed. Cervical conical resection can leave the uterus, but it has been reported that subsequent pregnancy increases the risk of miscarriage, premature birth, and caesarean section.
For stage IA1, simple total hysterectomy is basically recommended.
In stage IA2, radical hysterectomy or quasi-extensive hysterectomy + pelvic lymph node dissection is performed.
Radical hysterectomy, radiation therapy, or simultaneous chemoradiotherapy is recommended for stages IB and II. After surgery, if there is a high risk of recurrence, simultaneous chemoradiotherapy or radiation therapy may be given as postoperative adjuvant therapy.
Simultaneous chemoradiotherapy is the first choice for stage III or stage IVA.
In stage IVB, systemic treatment by chemotherapy (anticancer drug treatment) is the main treatment.
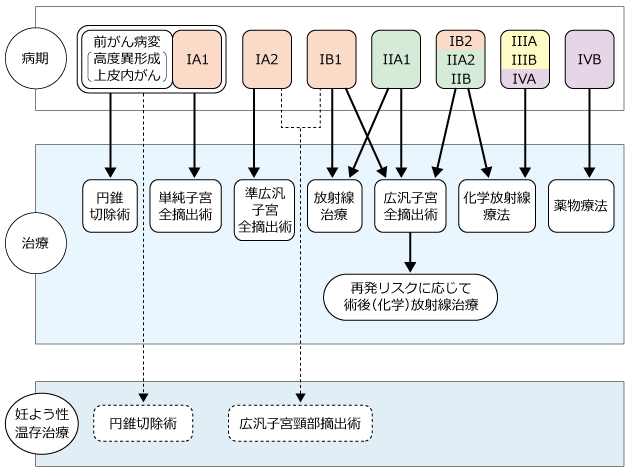
Reprinted from "National Cancer Center Cancer Information Service" https://ganjoho.jp/public/cancer/cervix_uteri/treatment.html
Based on the Japanese Society of Gynecological Oncology, "Cervical Cancer Treatment Guidelines 2017 Edition," p.24-28 (Kanbara Publishing)
Reprinted from "National Cancer Center Cancer Information Service" https://ganjoho.jp/public/cancer/cervix_uteri/treatment.html
▶当院での治療について
①手術療法
各々の術式に対して、開腹手術もしくは腹腔鏡下手術を適応に応じご提案しております。
広汎子宮全摘出術に関しましては、日本産科婦人科学会が定める“子宮頸癌に対する腹腔鏡下広汎子宮全摘出術登録施設”に当院は登録されております。
なお、現在当院では妊孕性温存を目的とした広汎子宮頸部摘出術は、現在行っておりません。
② Radiation therapy
Radiation Oncology, we perform external irradiation (irradiation from outside the body). We will introduce other hospitals for intracavitary irradiation performed by inserting special instruments into the uterus and vagina.
③ Simultaneous chemoradiotherapy
Intracavitary irradiation is performed at another hospital, but treatment is performed outpatiently or inpatiently.
④ Chemotherapy (anticancer drug treatment)
It is performed as preoperative and postoperative adjuvant therapy.
Subject in charge
- Head and neck cancer
- lung cancer
- Malignant pleural mesothelioma
- Liver cancer
- Pancreatic cancer
- Colorectal cancer
- Bladder cancer
- Prostate cancer
- Brain tumor
- Thyroid cancer
- Esophageal cancer
- Breast cancer
- Gastric cancer
- Kidney cancer
- Renal pelvis cancer / ureteral cancer
- Ovarian cancer
- Endometrial cancer
- Cervical cancer
- Skin cancer
- Cancer of unknown primary

