liver cancer
Liver cancer treatment at our hospital
At our hospital, pre-treatment diagnosis and treatment plans are thoroughly discussed in a joint conference between the Gastroenterological Surgery, Gastroenterology and Hepatology, and Diagnostic Radiology. Based on treatment guidelines, we discuss treatment plans with each patient, taking into account their individual condition, values, and wishes. In addition, hepatocellular carcinoma is prone to recurrence, and may require multiple treatments over the patient's lifetime. Rather than short-term treatment, we choose a plan that will allow treatment to proceed favorably in the future (e.g., pursuing a surgical plan that leaves as much remnant liver as possible during liver resection).
What is liver cancer? (causes, development, progression, etc.)
Liver cancer refers to cancer that develops in the liver, and can be broadly divided into primary liver cancer that develops in the liver itself, and metastatic liver cancer that has metastasized to the liver from other organs (such as the stomach or large intestine). Primary liver cancer can be further divided into hepatocellular carcinoma, cholangiocarcinoma, and others depending on the cells from which it originates, but hepatocellular carcinoma accounts for 95% of all cases, making it the most common type of cancer, so when people generally say liver cancer, they are referring to hepatocellular carcinoma.
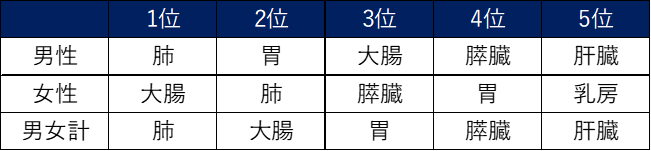
A characteristic of hepatocellular carcinoma is that it is caused by chronic liver damage or cirrhosis. 80% of cases are hepatitis caused by hepatitis B or C viruses, but in recent years, other chronic liver damage (alcoholic liver disease and non-alcoholic steatohepatitis (NASH)) has been on the rise. It is known to be a cancer that is prone to recurrence, and even after long-term survival after diagnosis, recurrence and repeated treatment are often observed. It is the fifth most common cause of death after lung cancer, colorectal cancer, stomach cancer, and pancreatic cancer.
Cancer deaths by site in 2018
▶肝細胞がんの進行度と肝予備能
肝細胞がんがどの程度進行しているかを表すのが、病期(ステージ)といわれるもので、StageⅠ~Ⅳで分類されています。肝臓がんのステージは、がんの局所進行の程度(大きさ、数、大きさ、周囲脈管への広がり)と 転移の程度 の組み合わせにより決定されます。
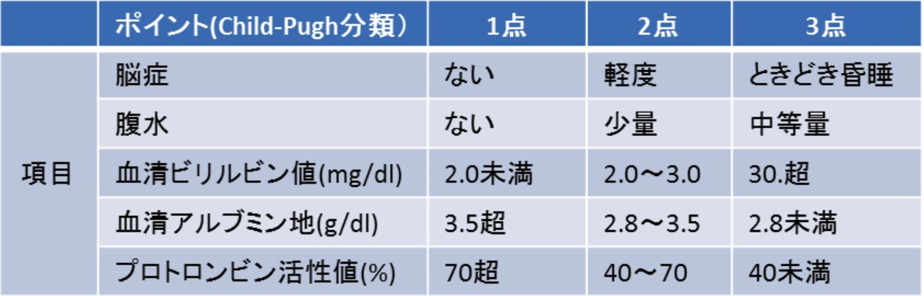
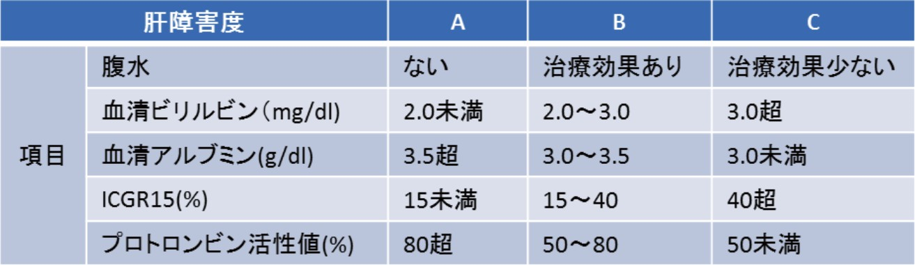
In addition to the stage of hepatocellular carcinoma, hepatic reserve (how damaged is the liver and how much capacity is available) is also a major factor in determining treatment. As described below, if hepatic reserve is sufficient, treatments that have a major impact on the liver and body (e.g. major liver resection) are possible, but if hepatic reserve is insufficient, treatment options are limited. The main evaluation methods used are the Child-Pugh score and liver damage classification.
☞Hepatocellular carcinoma stage
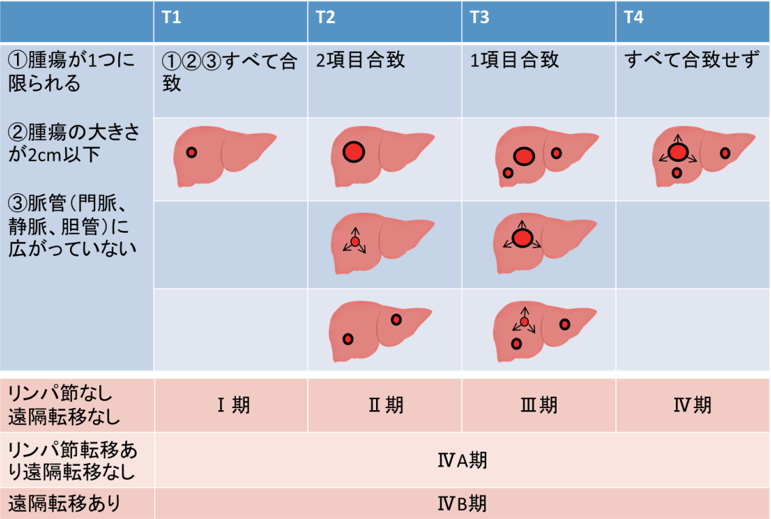
Reprinted with some modifications from "Clinical and Pathological Guidelines for Primary Liver Cancer, 6th Revised Edition" p.26 (Kanbara Publishing) compiled by the Japan Liver Cancer Study Group
☞ Indicators of hepatic reserve: Child-Pugh score and liver damage
Child-Pugh score
The following items are calculated and the total score is used to classify the grade: 5-6 points: A, 7-9 points: B, 10-15 points: C
Liver Damage Classification
Diagnostic method
The general flow from diagnosis to treatment is as follows.
0225-5.jpg)
□Blood tests
It is used to confirm the location and characteristics of the tumor and evaluate the condition of the liver.It may be used as a screening test for patients with a history of viral hepatitis.
□Ultrasound examination
It is used to confirm the location and characteristics of the tumor and evaluate the condition of the liver.It may be used as a screening test for patients with a history of viral hepatitis.
□ CT scan
X-rays are used to take cross-sectional images of the body.Local progression of hepatocellular carcinoma is evaluated, and the presence or absence of metastasis is determined. For accurate diagnosis of pancreatic cancer, examinations using contrast agents are mainly performed.
MRI examination
This is an examination that takes cross-sectional images similar to a CT scan, but it uses a strong magnetic field instead of X-rays.
This is the most useful test for differentiating tumors similar to hepatocellular carcinoma. As with a CT scan, a special contrast agent is used to observe the lesion in detail.
Method of treatment
There are many different treatments for hepatocellular carcinoma, but the most appropriate treatment is selected for each individual patient by weighing the state of the cancer (stage of disease, etc.), hepatic reserve function, and the patient's physical condition. Shown below is the treatment algorithm proposed in the domestic clinical guidelines. You can see that indices of hepatic reserve function, along with the state of hepatocellular carcinoma, have a significant impact on determining the treatment plan.
Treatment algorithm
0309-6.jpg)
Reprinted with some modifications from "Liver Cancer Treatment Guidelines 2017 Revised Edition" edited by the Japan Society of Hepatology, 2020, p. 70, Kanehara Publishing
□ Surgery for hepatocellular carcinoma
(1) Liver resection
Surgery for hepatocellular carcinoma is a "hepatectomy" in which a certain area of the liver is removed to remove the tumor. Because the cancer is removed from the body, it is the most reliable method compared to other treatments. However, the liver is an organ essential for sustaining life, and there is a limit to the amount of liver that can be resected. If the volume of the remaining liver falls below the amount needed to sustain life, there is a contradiction in that even if all the cancer is removed, it can be life-threatening (postoperative liver failure). In patients with reduced hepatic reserve, the amount of liver that can be resected is even smaller in order to prevent postoperative liver failure.
As mentioned in the treatment algorithm above, hepatocellular carcinoma suitable for liver resection is basically one that has not metastasized to any organs other than the liver and has three or fewer tumors. The actual surgical procedure is determined based on the balance between the planned amount of liver resection and liver reserve function, including whether surgery is possible or not.
web掲載内容-4-1.jpg)
☞ Complications of surgery
Hepatectomy for hepatocellular carcinoma is relatively safe when the resection volume is small, such as partial resection, but when the resection volume is large, there is a possibility of postoperative liver failure and serious complications such as death related to the surgery (mortality rate within 90 days after surgery: 2.7% for 1 segment resection, 3.9% for 2 segments). For this reason, it is important to carefully consider the surgical procedure (including whether or not the surgery can be performed) before the surgery. In addition to the complications of general abdominal surgery, liver resection can also cause complications specific to liver resection, such as leakage of bile, a digestive fluid synthesized in the liver, from the resected surface of the liver (bile fistula).
(2) Laparoscopic liver resection
Laparoscopic surgery is a procedure in which a camera and instruments are inserted through a hole in the abdomen and the surgeon watches a monitor. Compared to open surgery, it is known that the wounds are smaller and the burden on the body is less. Not all patients are suitable for laparoscopic liver resection, but we actively perform it when possible depending on the location of the cancer and the surgical procedure.
(3) Laparoscopic liver resection using ICG fluorescence imaging
By injecting a drug called Indocyanine green (ICG), the fluorescent properties of ICG can be used to stain the liver during surgery, making it possible to identify the area to be resected. In recent years, laparoscopic liver resection using ICG has become increasingly common, and our department was one of the first to adopt it and use it during surgery.
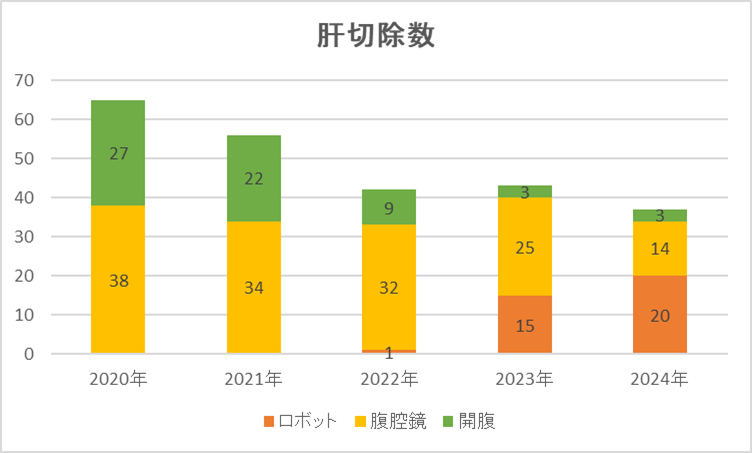
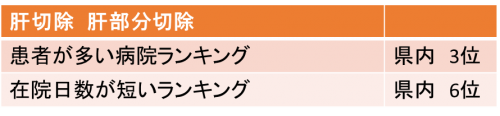
☞ Surgery results
The figures below show the number of liver resections and the ratio of laparoscopic surgeries performed at our hospital. We have one of the highest numbers of surgeries in the prefecture, and in recent years the proportion of laparoscopic surgeries among all surgeries has been increasing. Another feature of our hospital is the short length of stay after surgery, and in 2018 data we were the second highest in Kanagawa Prefecture.
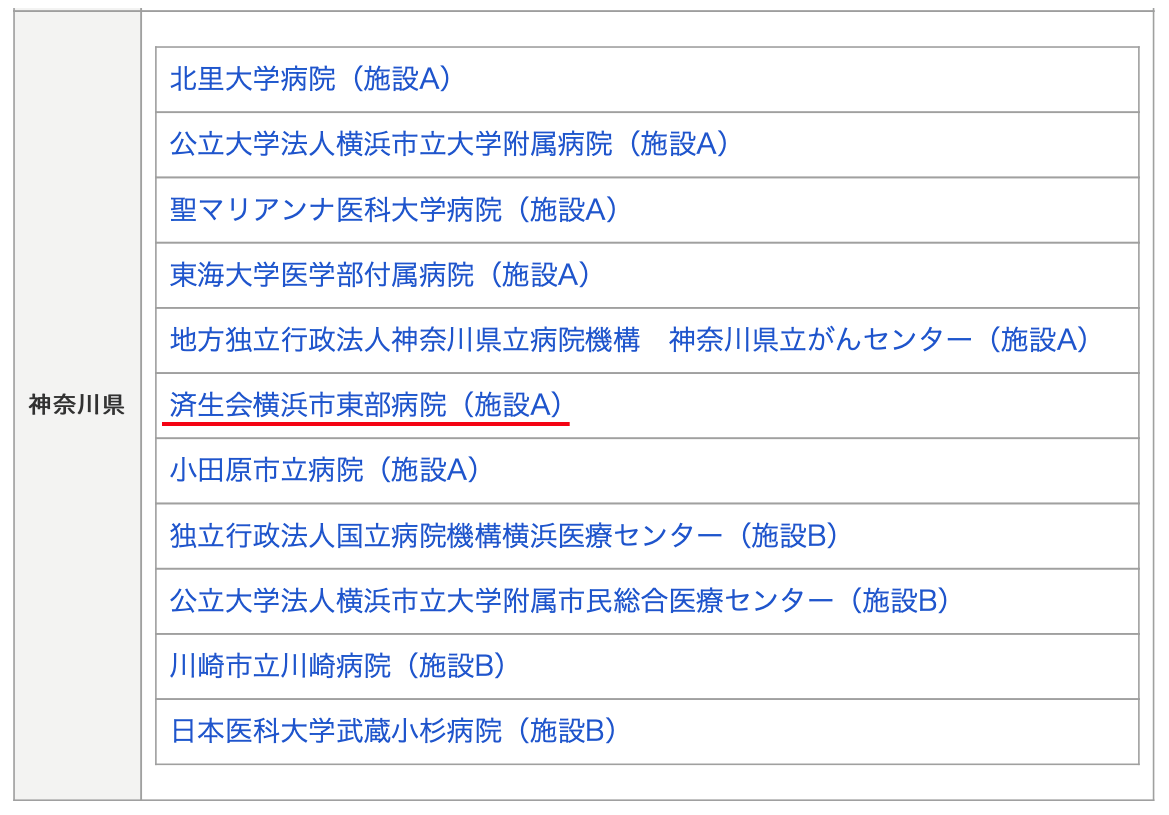
☞ Features of our hospital: Highly skilled specialist certified facility
It is known that in highly difficult hepato-biliary-pancreatic surgeries, including surgery for hepatocellular carcinoma, the mortality and complication rates associated with surgery are lower in facilities with a larger number of surgical cases (high-volume centers). Our hospital has been certified as an "Advanced Skills Specialist Certified Training Facility A" by the Japanese Society of Hepato-Biliary-Pancreatic Surgery, and is one of the leading high-volume centers in the prefecture. In Kanagawa Prefecture, only seven facilities, including our hospital, the prefectural cancer center, and university hospital, have been certified.
0309-9.jpg)
□Medical treatment for hepatocellular carcinoma
Surgery is the most reliable method to completely remove cancer, but for patients who cannot undergo surgery due to the progression of cancer or poor liver function, medical treatment is used. In practice, radiation therapy (Cyberknife, etc.), catheter therapy (transverse arterial chemoembolization, etc.), chemotherapy (anticancer drug therapy, molecular targeted drugs), etc. are used. At our hospital, we propose treatment methods that are tailored to the nature of each patient's cancer, physical strength, and wishes. We also have Pharmacist outpatient clinic for patients undergoing chemotherapy, where Pharmacist explain the need for anticancer drugs, treatment plans, and side effects, and support patients so that they can continue their treatment in the correct way with peace of mind.
(1) Catheter therapy (transarterial chemoembolization: TACE)
In general, hepatocellular carcinoma has a rich blood flow in the hepatic artery, which supplies nutrients to the tumor. Transarterial chemoembolization (TACE) is a treatment that uses an intravascular catheter into the hepatic artery that nourishes the tumor, injects anticancer drugs, and then injects an embolic substance to embolize the nutrient artery, causing ischemic necrosis of the tumor.
(2) Cyberknife
Cyberknife is a robotic radiation therapy device that is expected to have an excellent effect on patients who cannot be irradiated with conventional methods. Cyberknife was introduced at our hospital in April 2011. It can be used for cancers in various fields, but at our hospital, in cooperation with Gastroenterology and Hepatology and Radiation Oncology, we combine surgery with Cyberknife to perform various treatments for liver tumors such as hepatocellular carcinoma.
Medical treatment results
There are various treatments for liver cancer, including surgery, ablation (radiofrequency), embolization (TAE), CyberKnife, and chemotherapy, so it is recommended that you receive treatment at a general hospital.
In addition, for difficult liver cancer surgery, it is recommended that treatment be performed by a specialist at a facility designated by the Japanese Society of Hepato-Biliary-Pancreatic Surgery under the Advanced Skills Specialist System. (Link: Japanese Society of Hepato-Biliary-Pancreatic Surgery) Our hospital is certified as a specialized facility, and treatment is performed by a specialist (Table 4). Our hospital is proactively introducing the less invasive "laparoscopic hepatectomy." Laparoscopic hepatectomy has been covered by insurance since April 2010, and there are many reports that compared to open surgery, there is less bleeding during surgery, the number of days spent in hospital after surgery is shorter, and there is no difference in long-term results, and it is now safely performed at many facilities. Furthermore, endoscopic surgery is performed at our hospital by a doctor certified by the Japanese Society of Endoscopic Surgery. (Link: Japanese Society of Endoscopic Surgery).
(Table 4) Training facilities of the Japanese Society of Hepato-Biliary-Pancreatic Surgery
Number of treatments at our hospital
The number of liver surgery cases at our hospital is increasing year by year (Table 5). We also have one of the largest numbers of cases in Kanagawa Prefecture, with few complications and short hospital stays (Table 6).
(Table 5) Number of liver surgery cases at our hospital
(Table 6) Number of liver surgeries and length of hospital stay at hospitals in Kanagawa Prefecture
(Link: Survey by the Hospital Information Bureau in 2015)

Subject in charge
- Head and neck cancer
- lung cancer
- Malignant pleural mesothelioma
- Liver cancer
- Pancreatic cancer
- Colorectal cancer
- Bladder cancer
- Prostate cancer
- Brain tumor
- Thyroid cancer
- Esophageal cancer
- Breast cancer
- Gastric cancer
- Kidney cancer
- Renal pelvis cancer / ureteral cancer
- Ovarian cancer
- Endometrial cancer
- Cervical cancer
- Skin cancer
- Cancer of unknown primary

